Effect of BRT with MEBT/MEBO on the Expression and Regenerat
作者:Rong Xiang Xu 出版社:KARGER 发行日期:In 2004INTRODUCTION
As an innovative therapeutic system in burns therapy, BRT with MEBT/MEBO has enjoyed wide clinical acceptance as part of a protocol including the topical drug ointment MEBO. This therapeutic system successfully solved four major clinical problems: pain, wound infection, progressive necrosis, and scarring in deep second-degree burns wounds. Recently, a new landmark innovation, the regeneration and replication of skin tissue in the subcutaneous fat tissue of full-thickness burns wounds, has been accomplished by this innovative protocol. We know that no stem cells remain in the basal layer of epidermis of deep second-degree and superficial third-degree burns wounds. Therefore, we investigated the source of the regenerative epidermal stem cells which makes the fatty layer burns wounds repair spontaneously. This study was designed to observe dynamic changes in the regenerative epidermal stem cells of deep burns wounds tissues using the immunocytochemistry method.
MATERIALS AND METHODS
Tissue samples were taken from both normal skin and burns wounds of the following 2 burns patients who received BRT with MEBT/MEBO treatment as first aid immediately after the burns incident.
Case 1: A 6-year-old boy was scalded by hot water on his back and both lower limbs with area of 33 % TBSA and depth of deep second-degree.
Case 2: A 24-year-old male sustained flame burns on his four extremities with an area of 25 % TBSA, and depth of deep second-degree and superficial third-degree.
Tissue samples of the injured areas were taken from wounds of the 2 patients at 24 h and on 4, 7, 14, 21 and 28 days postburn. The samples were placed in plastic tubes and frozen with liquid nitrogen immediately, then embedded in Tissue-Tek OCT Compound and frozen in liquid nitrogen. Sections of 10 m thickness were made in a constant freezing microtome.
Indirect immunofluorescence staining with a biotin-avidin DCS system was performed. The frozen section was incubated with 10% horse serum at 4oC for 20 min, then a diluted (1:20) solution of mouse anti-human keratin type 19 monoclonal antibody (the 1st antibody) was added and the mix was again incubated overnight at 4oC. Subsequent to washing with phosphate buffer solution, the section was added to 7.5 g/ml of biotinized horse anti-mouse IgG antibody (the 2nd antibody, Vector Laboratories, Burlingame, Calif., USA) and incubated at 4oC for one h. After another washing, 10 g/ml of biotin-avidin DCS (Vector Laboratories) was added and incubated at 4oC for one h. The section was rinsed and then mounted with glycerin containing 10% PBS and 1% p-phenylenediamine. A control section of normal skin was stained in the same way, but without adding the 1st antibody. All specimens were observed under an Olympus reflecting fluorescence microscope (Japan) and photos were taken using ASA400 KODAK films.
RESULTS
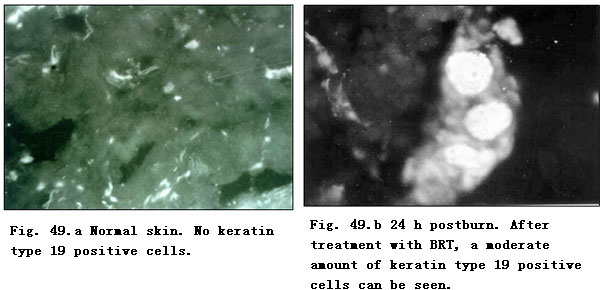
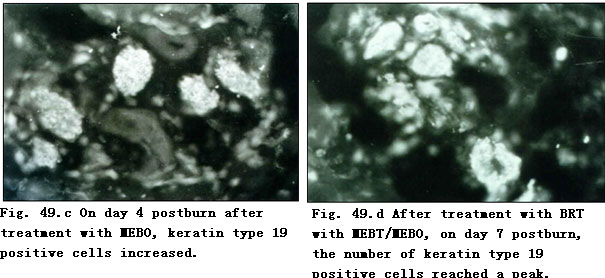
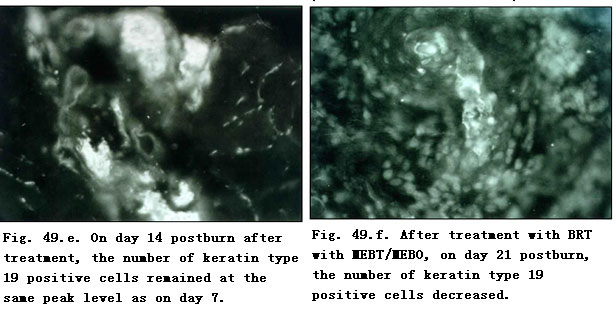
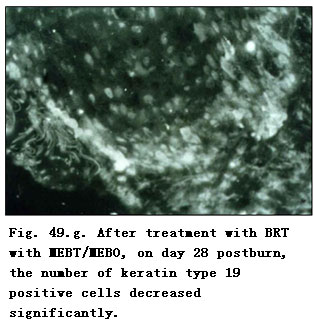
Immunocytochemical examinations were made on normal skin and burns wounds tissue sections treated with specific mouse anti-human keratin type 19 monoclonal antibody. The results revealed that in the normal control of both cases, there were few positive numbers of epidermal stem cells with keratin type 19 (Fig. 49. a). Wound tissue at 24 h postburn showed a moderate amount of positive epidermal regenerative stem cells (Fig. 49. b) and on day 4 postburn, the number of positive epidermal stem cells around the sweat gland, capillaries and hair follicles increased (Fig. 49. c). On days 7 (Fig. 49. d) and 14 (Fig. 49. e), epidermal stem cells containing human keratin type 19 continually increased and exceeded the level attained at day 4 postburn, before gradually reaching a peak level. Prior to days 21 (Fig. 49. f) and 28 (Fig. 49. g) postburn, the number of positive regenerative stem cells decreased to a certain level as the burns wounds progressed to healing. The observation showed that, after treatment with BRT with MEBT/MEBO, the proliferation status of the potential regenerative stem cell of the burns patients changed at a regular rate. We propose that regenerative stem cells may be the source of epidermal regenerative stem cells. The glowing fluorescent cells found observed under the microscope represented the potential regenerative stem cells in the wound tissues of deep second- and superficial third-degree burns. After treatment with MEBO, these stem cells may aid the deep partial thickness burns wounds to heal without scar formation and aid the superficial full-thickness burns wound to regenerate skin while healing spontaneously.
CONCLUSION
BRT with MEBT/MEBO promotes the activation and proliferation of epidermal regenerative stem cells in the residual viable tissue of superficial full-thickness burns wounds, and these stem cells play a unique role in the spontaneous wound healing of deep burns.
DISCUSSION
Research on the cell cycle has revealed that cell division is closely related to physiological regeneration and wound repair[1-11]. Some cells stay at phase Go or G1 for a long time and will not proliferate unless the condition becomes favorable. But some cells can undergo continuous division yielding daughters destined to differentiate to mature cells, while others retain their ability to continuously proliferate. These are termed “stem cells”. Stem cells in the basal layer of the epidermis are capable of proliferating continuously. Newly proliferated cells move upwards until reaching the deep area of the stratum spinosum layer, where they replicate two or three times before losing their proliferative abilities.
In deep second- and third-degree burns wounds, the whole epidermis and deep part of dermis are damaged so all resident stem cells in the basal layer of epidermis are destroyed. The residual viable mesenchymal cells around the hair follicles, sweat glands and capillaries in subcutaneous tissue may provide a source of available regenerative epidermal stem cells. These stem cells can synthesize specific cellular keratin type 19, and therefore can be identified by immunocytochemically. In this study, anti-human keratin type 19 monoclonal antibody was used. With the biotin-avidin DCS system and the indirect immunofluorescence technique, specific and exact detection of residual epidermal regenerative stem cells in the subcutaneous tissue of deep second- and superficial third-degree burns wounds is accomplished. We observed the number of potential regenerative stem cells with the positive label of human keratin type 19 reaching the peak level on 7 - 14 days postinjury in burns wounds treated with BRT with MEBT/MEBO. The immunofluorescent cells were epidermal stem cells, which induced the fatty layer burns wound to repair spontaneously. Therefore, we conclude that BRT with MEBT/MEBO treatment activates the dormant potential epidermal regenerative stem cell to proliferate, thereby ensuring the spontaneous repair and healing of deep burns wounds without scar formation. BRT with MEBT/MEBO treatment eliminates the lifetime of pain caused by the hyperplastic scars of patients with deep burns.
After transformation and differentiation, the epidermal regenerative stem cells can yield cells capable of synthesizing other types of keratin, i.e. keratin type 9 and 16. These cells still have the ability of transformation and can transform into the cells capable of synthesizing harder keratin ---- types 1 and 10. These are the typical types of keratin contained in mature epidermal cells. This finding proved that MEBO has the effect of promoting the activation, proliferation and transformation of epidermal stem cells.
It has been reported that when the cells are awoken from their dormant phase, the first activated protein is cyclin D. We know that cyclin D can only be expressed after being stimulated by growth factors. For eukaryotes, cells at phase G1 can either enter into the proliferation state or withdraw from the cell cycle. The main regulator of the phase G1 limiting point is the cyclin D1/CDK4 complex. In order to further investigate the mechanisms of the effect of BRT with MEBT/MEBO, we will continue our research on the gene regulation for the proliferation cycle of epidermal regenerative stem cells.
REFERENCES
1. Xu RX: Conspectus of Chinese moist burn therapy. Chin J Burns Wounds Surface Ulcers 1996; 8: 1-7.
2. Zhao JX: Experience with MEBT/MEBO in treating burn wounds. Chin J Burns Wounds Surface Ulcers 1999; 11: 16-17.
3. Xiao M: Clinical observation on MEBT/MEBO promoting severe burn wounds to regenerate and recover. Chin J Burns Wounds Surface Ulcers 1999; 11: 18-20.
4. Xu ZL, Parker SB, Minkoff R: Distribution of type IV collagen, Laminin, and fibronectin during maxillary process formation in the chick embryo. Am J Anat 1990; 187: 232-236.
5. Grana X, Reddy EP: Cell cycle control in mammalian cells: role of cyclins, cyclin dependent kinases (CDKS), growth suppressor genes, and cyclin-dependent kinase inhibitors (CKIS). Oncogene 1995; 11: 211-215.
6. Fuchs E, Green H: Multiple keratins of cultured epidermal cells are translated from different MRNA molecules. Cell 1979; 17: 573-577.
7. Lindberg K, Rheinwaid JG: Suprabasal 40 Kd keratin (K19) expression as an immunohistologic marker of premalignancy in oral epithelium. Am J Pathology 1989; 134: 89-98.
8. Bartek J, Bartkova J, Schneider J, et al: Patterns of expression of keratin 19 as detected by monoclonal antibodies in human breast tissues and tumors. Int J Cancer 1985; 36: 299-306.
9. Cohen IK, Mc Coy BJ: Wound Healing; in Goldsmith IA, ed. Biochemistry and physiology of the skin. New York, Oxford University Press, 1983, vol. 1, pp 462-474.
10. Zhang SQ, Wang YC (eds): Cell Cycle Control: Tendency of Cell Biology. Beijing, Beijing Normal University Press, 1996, vol 1, pp 46-60.
11. De Cherney AH, Dougherty WR, Rodgers KE, et al: Expression of cyclin protein after thermal skin injury in a guinea pig model. J Burn Care Rehabil 1997; 18: 292-296.