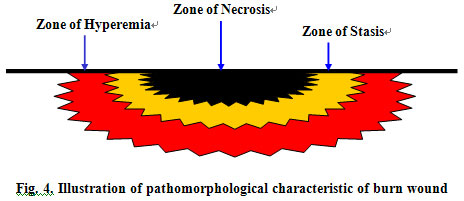
Pathogenesis Focus of Burn Wound
作者:Rong Xiang Xu 出版社:KARGER 发行日期:In 2004Following thermal injury, skin undergoes three injury phases in pathogenic order: physical injury, biochemical injury, and rejection response of necrotic tissues.
1. Physical Injury Phase: This includes direct and indirect physical injury. Immediately following skin surface exposure to thermal source, the resultant direct injury leads to necrosis of interface skin, which is called “direct physical thermal injury”. Although the thermal source causing the direct injury is removed, the heat does not dissipate from the skin immediately. The residual heat continues to produce a cumulative thermal effect which causes secondary thermal injury to the skin. This secondary trauma usually persists for 6~12 h. This is called “indirect physical injury phase”.
2. Biochemical Injury Phase: Local biochemical injury begins within 1 hour of the thermal insult and lasts for up to 72 h post-burn. This persists through the thermal biochemical reaction phase and the biochemical inflammatory reaction phase on the time order. At 1~2 h post burn, there is a significant increase in capillary permeability occurring in the injured, though still viable tissues, contiguous with the necrosis caused by direct thermal injury. This results in exudation of intravascular fluid toward the wound surface and interstitial space while tissue ischemia is occurring. Simultaneously, the injured but viable tissues and cells in the area of lesion develop edema due to metabolic disorder. At this time, the permeable capillaries release plenty of chemical substances which not only locally aggravate the injury itself and damage the peripheral uninjured areas, but also may subsequently result in systemic injury. Although it is not quite clear what these chemical substances are, they appear to include histamine, 5-HT, hydrogen ion, kinin and bradykinin, etc. This phase is called the “thermal biochemical reaction phase”. About 2 h later, thermal biochemical reaction continues to affect the viable tissues in the injured area to cause a series of inflammatory reactions. The initiation of such an inflammatory pathological reaction in the injured area may result in the full spectrum of pathological injuries. For instance, inflammatory reaction activates the blood coagulation system to induce progressive thrombosis of the microcirculation, which may cause necrosis of the injured but viable tissues and may also result in ischemic and anoxic necrosis of the surrounding uninjured tissues. This process may last for 72 h postburn and is called the “biochemical inflammatory reaction phase”.
3. Reject Reaction of Necrotic Tissues: At 72 h postburn, the wound tissue comes into a phase of rejection reaction, which is a response of the viable tissues due to disintegration of necrotic tissues and cells in the interface of the lesion area. Usually mixed and extensive, this reaction process primarily includes three pathogeneses: (1) the disintegration of necrotic histiocytes in the injury interface; (2) the regeneration of viable histiocytes in the interface of the lesion area; (3) microbial infection in the injury interface. Besides an inflammatory reaction, disintegration of necrotic histiocytes may induce cell liquefaction in the injury interface and, more importantly, the accumulation of cell liquefied products continues the aggravation of the injured tissue. Meanwhile, the residual viable tissues in the injury interface begin instinctive regeneration when disintegrated tissues develop into a destructive substance unfavorable to the environment of cell regeneration, thereby inducing serious inflammation. The combination of the two above pathogeneses disturbs flora residing in the skin and causes the destruction of microbes in the injured area, both of which further aggravate damages and may result in systemic injury at any time. This process is called “rejection injury of necrotic tissues”, and is the last primary injury of a burn wound.