Standardized Local Treatment of Burns Wounds
作者:Rong Xiang Xu 出版社:KARGER 发行日期:In 2004To help facilitate the understanding of a variety of burn treatment techniques, 3 cases were compared at the following three clinical procedures: treatment of burnt skin, healing and closure of wound, and need for reconstruction after wound healing.
Case 1: Surgical Excision and Skin Grafting Burns Therapy
Background Information
A 23-year-old male was burned when fire burned his cotton clothes ignited by steel residue at his workplace. Immediate antishock management was administrated at the factory clinic. At 4 h postburn, the patient was transferred and arrived at the hospital 7 h 20 min later. Upon arrival, initial assessment revealed that the patient suffered severe burns, including face and both auricles, anterior neck, both hands, chest, abdomen, left thigh and both legs; wound showing leather-like; dendritic vascular embolism. His vital signs included: T: 35.9 C, P: 44/min, R: 32/min and BP: unmeasurably low. The patient developed hypovolemic shock postburn which was complicated by inhalation injury.
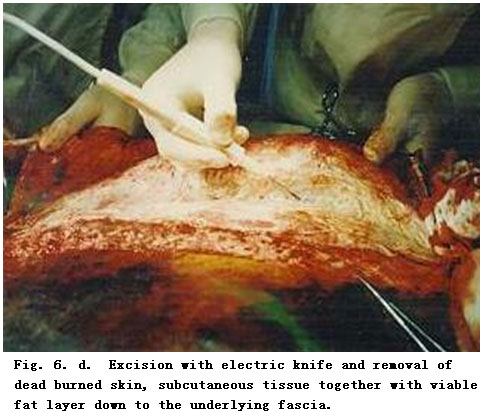
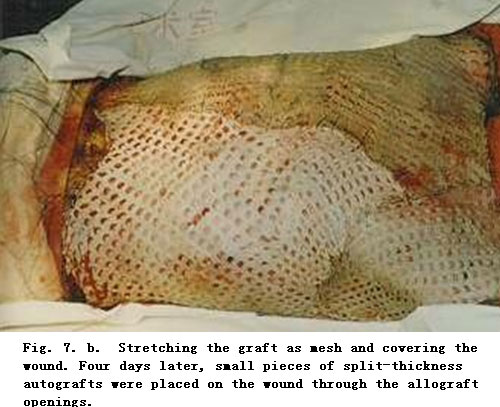
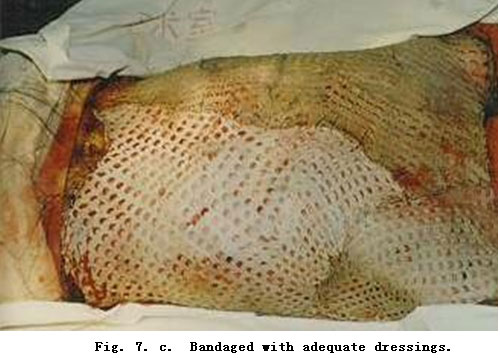
On admission, rapid fluid resuscitation was started to correct shock and tracheotomy was performed to improve ventilation. Escharectomy was then performed on the third-degree wounds of the left forearm and both legs to relieve pressure and improve blood circulation at the extremities. Superior vena cava puncturing and right cardiac floating catheterization were performed to monitor heart function. On day 2 postburn, surgical eschar excision to the underlying fascia and micro-particle autografting was performed on the extremities. On day 6, the patient received eschar excisions on the chest and abdomen, on which evenly holed allograft sheets were applied. Four days after the operation (day 10 postburn) small pieces of split-thickness autografts were placed on these wounds through the openings of the allograft. The patient developed severe Pseudomonas septicemia, and became comatose with low body temperature for 1 week. Septicemia was well controlled after intensive care. After that, repeated skin grafting was performed 9 times and most of the wounds healed. On day 43 postburn, corneal ulcer in the left eye occurred and was treated with eye drops and retrobulbar injection. Corresponding measures were taken to prevent stress ulcer, control infection and prevent pulmonary complications. The length of hospitalization was 70 days.

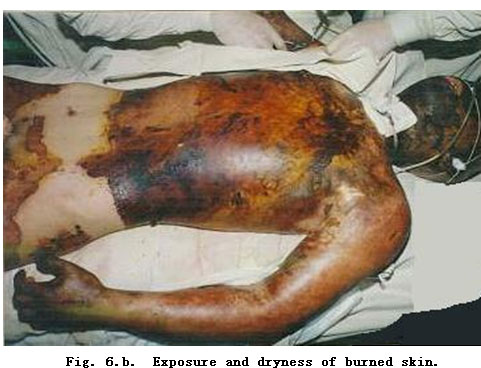

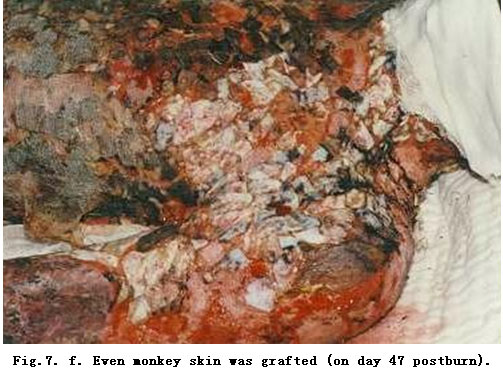
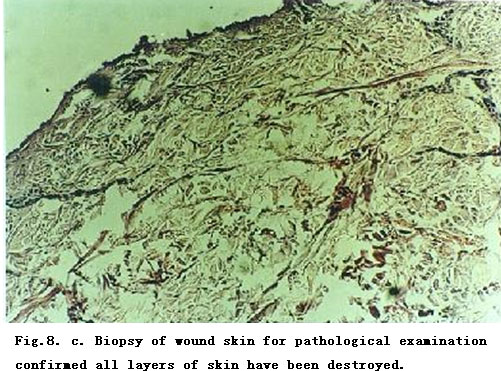
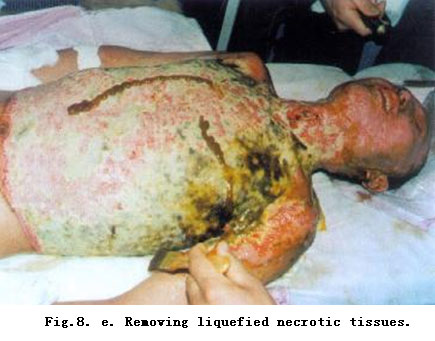
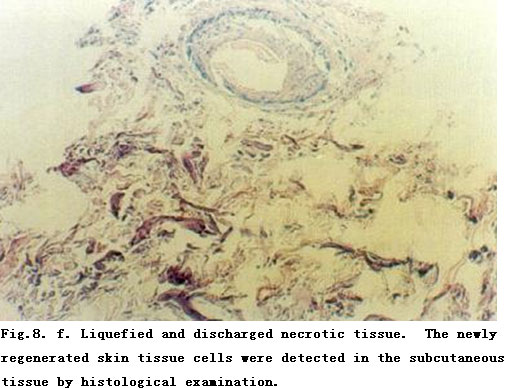
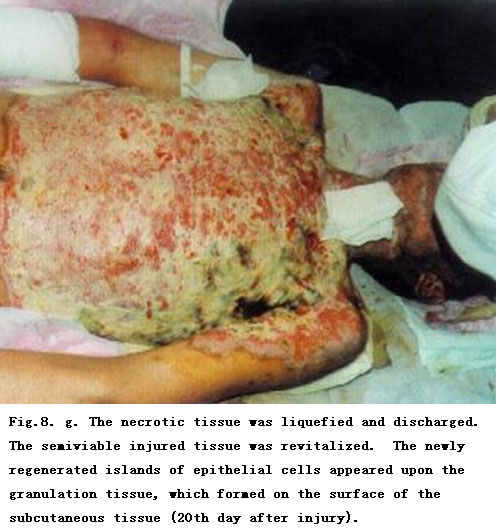
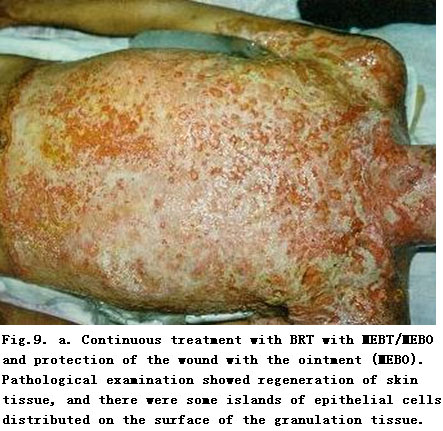
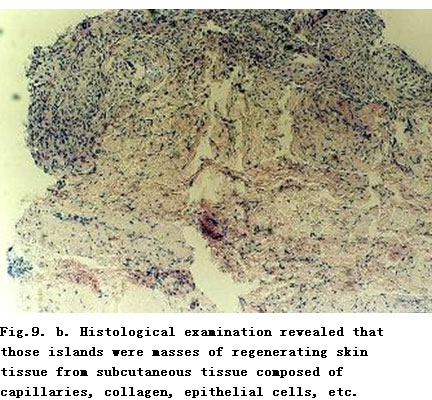
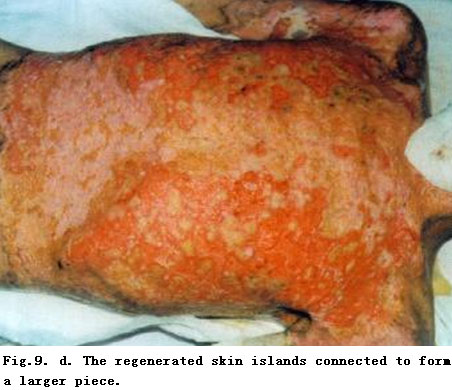
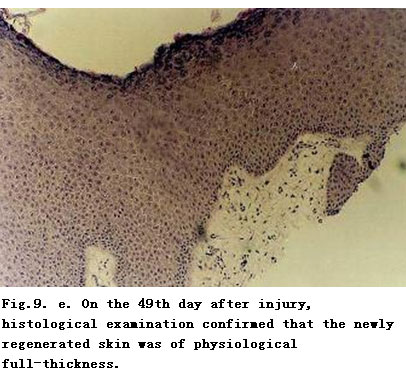
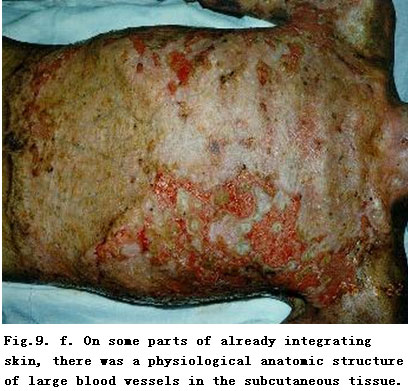
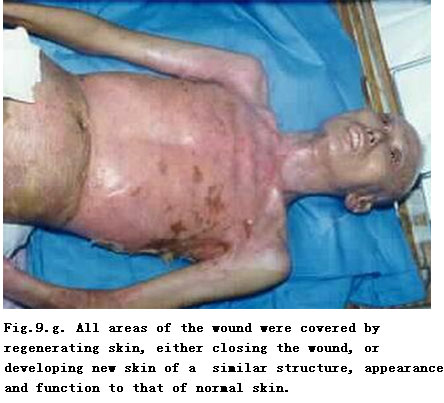
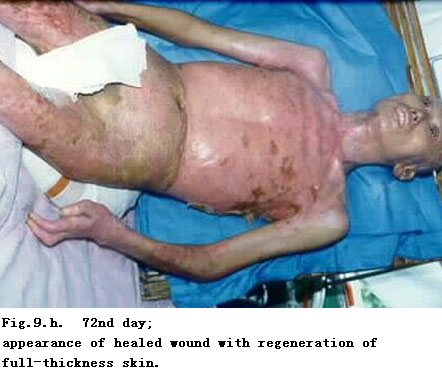
Procedure and Result (fig. 6, 7) disabled. Case 2: Burns Regenerative Medicine and Therapy (BRT with MEBT/MEBO) On admission, the patient was in a critical state and in shock. The extensive deep burns wounds were covered by cement powder. He had inhaled cement and his nasal hairs were singed. He suffered from respiratory abnormality and hoarseness. Tracheotomy was performed immediately. BRT with MEBT/MEBO treatment and cultivating technique was started on the wound and systemic comprehensive management begun. Histological examination of the wound skin showed third-degree burns. On day 30 postburn, liquefaction and discharge of wound necrotic tissues were finished. On day 49 postburn, newly regenerated skin was present on the wounds. Ten days later large sections of regenerated skin appeared on the wounds and all wounds had healed completely on day 72 postburn. One year later, follow-up showed the patient free of disablement, capable of independent viability and no need of reconstruction. Third step: Reconstruction after wound healing. Ed. Note: In the spirit of brevity, the author has offered photographic documentation of 2 cases only. However, the author has documented hundreds of similar cases and for those who would appreciate reviewing that extensive photographic library, we refer you either to the literature of to www.mebo.com. 1). Background Information matrix makes CEA susceptible to infection, shearing forces and limits their incorporation into the burn wound. A cultured composite autograft (CCA) has been developed recently in which autologous keratinocytes and fibroblasts are surgically harvested from the burns patient’s normal skin. These components are proliferated and then combined to form an epidermal and dermal matrix which grows into confluence and is then applied to the leasion. Standard wound coverage techniques as well as CCA technology were utilized for successful wound closure in a 12-year-old female with an 81 % third-degree burn. After fascial excision and allograft coverage, autografts were placed on her posterior burns and then 7,500 cm2 of CCA was placed onto her anterior thorax, abdomen and lower extremities. Sixty percent of the burns was covered with CCA resulting in a success rate of 40 %. No evidence of infection was noted, even in areas where CCA failed, although in those areas random epithelialization appeared to occur which then seemed to facilitate autograft placement. Early debridement and allografting followed by conventional autografts and CCA placement may provide an effective skin coverage strategy in patients with extensive deep burns. 2). Procedure and Result: Disablement and disfigurement. Reconstruction was required. Pictures of the treatment procedure are not available here as copyright is concerned. See Burns 1999, 25 (8): 771-779 for details.
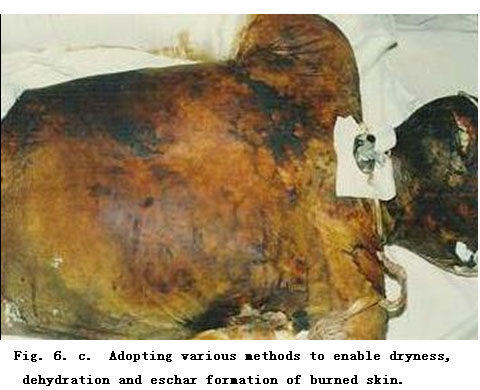
First Step: Treatment of Burned Skin
Dryness and debridement of eschar replaced the burn wound by a surgically included traumatic wound with neither burnt tissue nor skin tissue.
Second Step: Healing and Closure of Wound
Third Step: Reconstruction after Wound Healing
During a period of 14 months, nine surgical reconstructive operations were performed. However, disablement and disfiguration still presented.








Background Information
A 35-year-old male sustained scalds by 1,000 C hot cement and flame burns secondary to a cement kiln collapse accident at 8:30 p.m. on April 12, 1996. He was admitted to the hospital at 4.5 h post injury. The initial assessment showed: (1) Burn-blast combined injury; (2) Extensive deep burns (85 % TBSA); (3) Severe inhalation injury; (4) Shock; (5) Open multiple fractures on both feet.
No need.
+
Case 3. Surgical Excision and Cultured Composite Autograft Therapy
Cultured epithelial autografts (CEA) have been used as an adjunct in the surgical management of extensive thermal burns. Unfortunately, the lack of a dermal