A Comparative Study on the Antishock Effect Between BRT with
作者:Rong Xiang Xu 出版社:KARGER 发行日期:In 2004INTRODUCTION
Many clinical reports have shown that treatment with BRT with MEBT/MEBO reduces the volume of fluid loss, thereby minimizing the shock effect in the treatment of extensive burns. Using an 8-hour postscald rabbit model, the authors designed a comparative study between this therapy and conventional dry-exposed burns therapy in order to evaluate the antishock effect of BRT with MEBT/MEBO.
MATERIALS AND METHODS
18 healthy adult male and female rabbits weighing 2.0~2.6 kg were divided randomly into group A (treatment with MEBO, n=9) and group B (dry exposure, n=9). The animals were anesthetized with 3 % pentobarbital sodium 30 mg/kg intravenously via ear vein, intubated and then catheterized (left common carotid artery). The cannulae were connected with a multi-channel physiological recorder so that the respiratory rate (RR), heart rate (HR), arterial blood pressure (ABP) and electrocardiogram (ECG) were able to be monitored continuously. At 30 min after operation, when the above noted vital signs were stable, the anaesthetized animals’ backs were scalded with 75°C water for 20 s in order to produce consistent deep second-degree burns of 40 % BSA. The degree of tissue burn trauma was then verified by pathological examination. Next, the wounds of both groups were put under a 100 W incandescent light bulb at a distance of 50 cm. The wounds of group A were treated with MEBO applied at a thickness of 1 mm, and renewed every 2 h. The wounds of group B were washed with 0.1 % bromogeramine and normal saline. Additionally, both groups received the following total amount of fluid infusion in the first 24 h after injury (ml) = 40 body weight (kg) 2 (ml) plasma substitute + 40 body weight (kg) 2 (ml) balanced salt solution + 400 ml 5 % glucose solution. Half of the total amount was infused at a corrective rate during the first 8 h after injury.
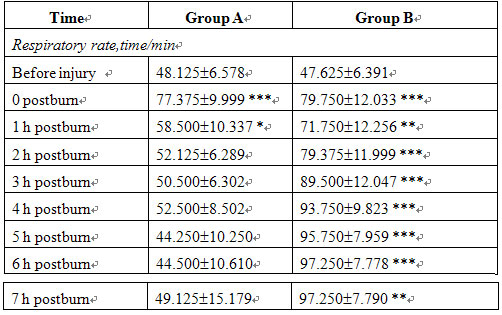
The RR, HR, ABP and ECG were measured at 5 min and at the end of each hour until the 8th hour after injury. Through the carotid artery catheter, blood samples were taken from 6 rabbits in each group at 5 min and 8 h, respectively. A type NXE-1 viscometer was used to measure blood viscosity the at different shear rates. The wound tissues were sampled for pathological examination at the end of the experiment. The statistic analysis was derived from auto-control t test.
RESULTS
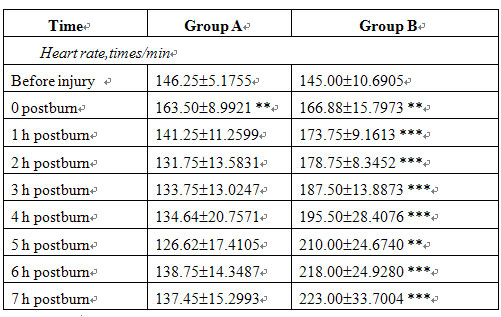
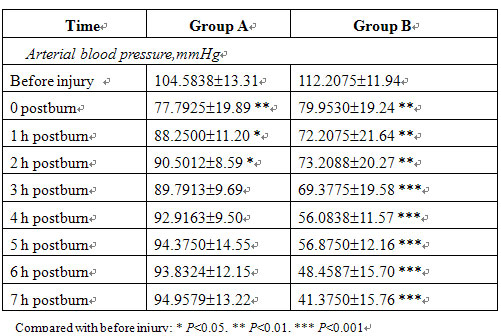
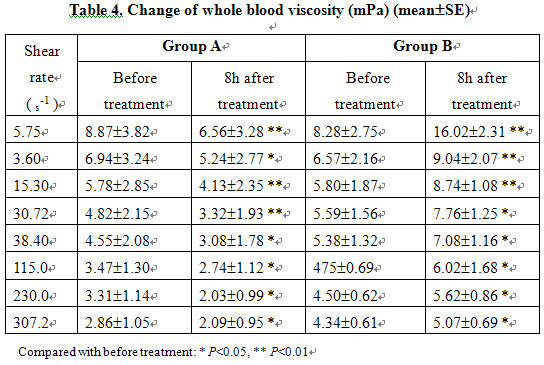
Before injury and at 5 min after injury, RR, HR and ABP were not significantly different between the two groups. In group B, RR and HR increased, ABP decreased progressively postinjury and the blood viscosity was raised markedly after treatment compared with that of before treatment. In group A, the MEBO-treated group, the RR, HR and ABP of all animals gradually recovered to the preinjury levels after treatment while blood viscosity decreased significantly (Tables 3, 4).
By contrast, 6 animals in group B developed ventricular premature beat at 4 h postinjury. One of them appeared apneic, required the rescue effort of artificial respiration and closed cardiac massage, but died 1 h later despite this. Another animal died at 8 h postinjury. These two deaths were the only fatalities in the study and both were from the non-MEBO-treated group. In group A, two animals developed occasional ventricular premature beats, but no death resulted. Upon gross inspection, wounds in group A were moist and supple with a pale red color and normal microcirculation. In group B, wounds appeared wizened with a layer of eschar at the surface, fluid congestion under the crust membrane and compromise in the microcirculation as seen by stasis and dark red flaking lesions. Pathomorphological examination showed epidermis defects and residual degenerative necrotic tissues in dermis surface only in group B. Furthermore, dramatic congestion and edema of the intradermis and a significant tortuosity and thrombosis of the capillary were also observed. By contrast, pathomorphological examination of group A showed swelling of the dermis, mild congestion with telangiectasia, infiltration of the small lymphocytes and a total absence of thrombosis.
CONCLUSION
Burns regenerative medicine and therapy (BRT) has antishock effects by the proposed mechanism of reduction of water evaporation from the wound surface, maintenance of a sufficient blood volume, decreasing blood viscosity, improving the local and systemic microcirculation, and reducing the absorption of burn toxins.
Table 3. Changes in respiratory rate, heart rate and arterial blood pressure (meanSE)
DISCUSSION
1. MEBO is Superior To Dry Expose Burn Therapy in Antishock Effect
The authors used rabbit model with the same area of second-degree scalds to be treated with the same antishock fluid resuscitation but different wound care management, i.e., MEBT/MEBO in group A and conventional dry-exposed therapy for group B. Measurement of HR, RR and ABP were made and the same statistic analyses indicated that animals in group A experienced a smoother shock period than those in group B. The ECG showed that 2 rabbits in group A developed ventricular premature beat (22.2 %) and the death rate was 0, compared to 6 rabbits with ventricular premature beat (66.6 %) and two deaths with a mortality of 77 % in group B. The results showed that treatment in group A was superior to that in group B with respect to antishock effect. In the management of extensive burns, BRT with MEBT/MEBO has proven itself to be the treatment of choice though questions remain regarding the precise protocols of fluid infusion in order to afford subjects the optimal volume for protection against shock
2. Mechanism of antishock effect of BRT with MEBT/MEBO.
Maintenance of Effective Blood Volume. For extensive burns, the permeability of local capillaries increases significantly with the majority of exudation of plasma-like fluid occurring in the first 2 h postinjury. Another increase in exudation then occurs during the 6~8 h postinjury. Furthermore, the sympathetic upregulation due to pain and nervousness may increase the water loss from evaporation of respiratory tract. All of above factors conspire to increase blood concentration, reduce effective circulating volume, and dispose the physiology toward hypovolemic shock. The base of MEBO includes sesame oil and beeswax. Sesame oil has minimal molecular weight and high lipophilic tendency that utilizes certain properties of its co-ingredient, beeswax, to resist rancidification and saponification. Therapeutic aspects of this sesame/beeswax base conspire to prevent evaporation of water from the wound site while isolating wound tissue from the outside environment. In addition, the application of MEBO to the wound has an immediate and much welcomed analgesic effect. Recall that pain-induced stress or anxiety and since many clinic reports have verified the effectiveness of MEBO as a potent analgesic, it is reasonable to assume that MEBO also reduces water evaporation from the respiratory tract. This study can be interpreted as confirmatory in that rabbits in group A received BRT with MEBT/MEBO treatment within 8 h postinjury and suffered less water evaporation than those in group B, indicating that an effective blood volume was maintained, thereby protecting them from hypovolemic shock.
To Improve the Microcirculation. Shock is a clinical syndrome mainly characterized by acute dysfunction of the microcirculation. In the clinical setting, symptoms include microvascular contraction, enhanced capillary permeability, endothelial cells injury and functional / morphological changes of blood cells, which may lead to thrombosis. Efforts should be made to reverse microcirculation dysfunction in the period 1~4 h postinjury through aggressive antishock therapy. Failure to do so can prove to be lethal. In this study, gross and micropathological examinations revealed unfortunate dryness of the wound, flaking of ecchymosis under the eschar, and tortuosity with thrombosis of capillaries in group B.
The presence of thrombosis postburn was associated with relatively sluggish blood flow, varied vascular structure, altered blood concentration and aggregation of blood cells. Excessive water evaporation from the wound sites magnified blood concentration and deteriorated microcirculation stasis, finally leading to dry necrosis. This cascade contributed to the obvious shock in group B animals. In contrast, wounds in group A appeared rubicund and moist with an absence of capillary microthrombi, and a normal blood circulation without coagulopathy. Accordingly, there were only slight symptoms of shock in group A. These differences may be attributable to the effect of BRT with MEBT/MEBO in improving microcirculation. By preventing water from excessive evaporation, this BRT method maintained effective blood volume. This relatively fast blood flow prevented the microcirculation from developing stasis and enforced effective perfusion. Additionally, as wound tissue remained moist, cell dehydration was minimized and the physiology resisted tendencies toward shock.
To Reduce Whole Blood Viscosity: Viscosity refers to the degree of friction of blood elements during fluid flow. Viscosity of the blood may be increased by the sympexis resulting from slow blood flow and/or aggregation of erythrocytes, and by increases of macromolecule proteins such as fibrinogen. Trappeiner was the first to propose that burns could cause a concentration of blood. Baxter also reported an increased viscosity of the blood in burns patients. It was observed that following a burn injury, plasma exudation and high concentration of blood might result in the above changes and therefore increase blood viscosity, as burn shock is aggravated by an excessive blood viscosity. The results of this study showed a significantly decreased viscosity of the blood at 8 h postinjury in group A compared to group B. This suggests that BRT with MEBT/MEBO reduces plasma exudation, minimizes aggregation of erythrocytes, improves blood viscosity and flow, and reduces sympexis, all of which significantly minimizes the risk of shock as compared to dryexposed burns therapy.
To Reduce the Resorption of Burn Toxins: When skin is burned, many new compounds called burn toxins are produced and absorbed into the circulation. Hunter and Rosenthal isolated a 12,000-14,000-dalton protein from burn exudates which contained peptide, polynucleotide, hexose and pentose. This protein inhibited cardiac muscle function and so they named it myocardial depressant factor (MDF). Mitsuyoshi found an increase of serum lipid peroxide (LPO) in burns patients which he proposed could cross-link with lipoprotein in serum to produce toxins. Mombnhko intravenously administered the rat purified burn toxin extracted via immunoadsorption. At 2 h postinjection, arterial blood pressure decreased from 1257 mmHg to 748 mmHg, suggesting that burn toxins reduced blood pressure to aggravate shock by inhibiting cardiac function. The results of this study showed an obvious decrease in blood pressure, 66.6 % of rabbits developing ventricular premature beats and 2 deaths in group B, which suggested a remarkable shock resulting from burn toxins. In group A, shock was minor with less burn toxins. One of three possible solutions put forward to counter burn toxins was the early excision and remove of burned tissue so as to prevent burn toxins from absorption, and therefore alleviate shock.
MEBO was applied to animals in group A at a standard dosage at room temperature. Two layers appeared on the wound surface subsequent to application, an ointment layer and a liquid layer. Warmed by the body temperature of the wound, the ointment layer became less viscous and attaining a relatively liquid form it mobilizes the necrotic tissue with the wound. MEBO then mixes with exudates, liquefies necrotic tissue and metabolic products to produce a conglomerate of lipophobic, whitish material which is propelled away from the wound. Thus, by converting the lipophilic necrotic debris into a lipophobic MEBO complex, the wound is cleansed via an automatic drainage process while neither irritating nor distressing to the viable wound tissues. This innovative process is superior to the excision of necrotic tissues and results in the advantage of a reduced absorption of burn toxins. In this way, MEBO reduces shock potential as it causes no decrease of blood pressure, no inhibition of cardiac muscle and no damage to the microcirculation. In contrast, conventional therapy involving dry-exposed burns therapy results in the drying of necrotic tissue, and an unhealthy absorption of burn toxins which increases the odds of shock and even death.